A study focused on patient experience offers a clearer picture of the most common side effects associated with two groundbreaking rTMS protocols.
The loss of her brother sunk lawyer Lisa Ridgway into a deep depression that was resistant to standard treatments. Open to alternative options, Ridgway received the novel repetitive transcranial magnetic stimulation (rTMS) therapy, which gave her hope and set her on a path to becoming a patient partner in a first-of-its-kind study led by Vancouver Coastal Health Research Institute researcher Dr. Fidel Vila-Rodriguez.
“Being involved in that study was very important to me because it can help to inform patients—from bench to bedside,” says Ridgway. “The approach taken for this study shows that patients come first.”
The non-invasive rTMS therapy involves applying a series of magnetic pulses to specific areas of the brain to stimulate and change the firing patterns of brain circuits. Shown in prior studies to be a successful first-line intervention for people with treatment-resistant depression, rTMS is believed to be able to rewire the brain to help relieve symptoms.
Depression—characterized by such feelings as emptiness, fatigue and suicidality—affects around 5.4 per cent of Canadians, and around 30-40 per cent will develop a form that does not respond to medication or counselling.
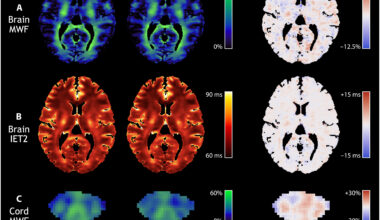
Vila-Rodriguez’s secondary trial—published in the journal, Brain Stimulation—is the first known study to compare the pain and side effects associated with two protocols of rTMS—intermittent theta burst stimulation (iTBS) and high-frequency left (HFL)—for treatment-resistant depression. iTBS is a newer protocol that delivers three bursts of magnetic pulses at a frequency of 50 Hz over the course of three minutes. HFL delivers pulses over the course of 37.5 minutes at a level of 10 Hz.
Vila-Rodriguez’s study reviewed data collected in the THREE-D trial that included 414 adult participants between the ages of 18 and 65 who randomly received either HFL or iTBS. Vila-Rodriguez’s research team found that reported pain severity decreased significantly over the course of treatment using both protocols, although iTBS was found to be more uncomfortable.
Participants who were older, female and had high anxiety levels also experienced more pain. Although, the greater the positive response to the treatment, the less pain patients reported experiencing, Vila-Rodriguez’s research found.
Patient perspective helps move research into clinical practice
Ridgway and Vila-Rodriguez initially connected through the social media platform Twitter after Ridgway posted about her experience receiving rTMS.
“When I first went through the treatment, I did not realize that there could be pain or side effects associated with the procedure,” recalls Ridgway. “I had very minimal side effects or pain. And, after several treatments, it became almost a meditative experience and quite relaxing.”
Ridgway’s journey soon led her into the realm of patient-oriented research, where she became involved in studies associated with mental illness and health care. Now a patient partner with Vila-Rodriguez’s NINET Lab, Ridgway provides essential insight into lived experience and patient perspective to help shape the user-friendliness of research materials.
“Since Lisa joined the NINET Lab as a patient-partner, staff and myself have all become more aware of the importance of translating research into clinical practice.”
Dr. Fidel Vila-Rodriguez
Vila-Rodriguez and the NINET Lab consulted with Ridgway on the language used in the study, along with an infographic that illustrates the study’s findings.
“When we produced the first draft of the paper, it read more like a standard science paper with a lot of technical terminology and clinical language,” recalls Vila-Rodriguez. “Lisa’s insights shifted the tone, enriching it with more functional information and plain language that put the people who will receive the treatment at the forefront.”
Vila-Rodriguez’s infographic will be printed off as a poster for installation in treatment rooms where psychiatrists and clinicians can reference them when describing rTMS and its common side effects.
Dr. Fidel Vila-Rodriguez is the director of the Non-Invasive Neurostimulation Therapies (NINET) Laboratory, a clinician-scientist with the Djavad Mowafaghian Centre for Brain Health and an assistant professor in the Department of Psychiatry at UBC. Lisa Ridgway is an advocate for patient-oriented research and mental health care issues. She currently collaborates with teams at UBC and the University of Victoria.
This story was originally published on the Vancouver Coastal Health Research Institute’s website.