The Lancet Neurology has published a dedicated Commission on the advances and persisting and new challenges in prevention, clinical care, and research in Traumatic Brain Injury (TBI).

Dr. Cheryl Wellington
The 2022 Commission has been produced by world-leading experts, including DMCBH member Dr. Cheryl Wellington, and will be presented to all Participants of the Collaborative European Neurotrauma Effectiveness Research in TBI project (CENTER-TBI) at their meeting in Antwerp, Belgium on September 30, 2022. This is an update to the first Lancet Neurology Commission on TBI, which was launched at the European Parliament in 2017. The 2017 Commission set out priorities and recommendations to address the challenges in TBI from the perspectives of policymakers, clinicians, and researchers. Since then, new knowledge has been generated by large observational studies, including CENTER-TBI and other studies conducted under the umbrella of the International Traumatic Brain Injury Research (InTBIR) initiative, designed as a coalition of funding agencies and scientists to advance the care for patients with TBI through collaborative efforts.
The Commission documents traumatic brain injury (TBI) as a global public health problem, which afflicts 55 million people worldwide, costs over US$400 billion per year, and is a leading cause of injury-related death and disability. TBI is not only an acute condition but also a chronic disease with long-term consequences, including an increased risk of late-onset neurodegeneration, such as Parkinson’s disease and dementia. Road traffic incidents (RTIs) and falls are the main causes, but their relative contribution differs between low- and middle-income countries (LMICs) and high-income countries (HICs). In LMICs, RTIs account for almost 3 times the number of TBIs as falls, whilst in HICs falls cause twice the number of TBIs compared to RTIs. These data have clear consequences for prevention.
Over 90% of TBIs are categorized as “mild”, but over 50% of such patients do not fully recover by 6 months after injury. Improving outcome in these patients would be a huge public health benefit. A multidimensional approach to outcome assessment is advocated, including a focus on mental health and post-traumatic stress disorder. Outcome after TBI is poorer in females compared with males, but reasons for this are not clear.
“The Wellington lab is honoured to have leadership roles in the International Initiative on Traumatic Brain Injury Research, The Canadian Traumatic Brain Injury Research Consortium, and the Canadian Concussion Network. Through these international and national efforts, our research program on blood biomarkers for TBI across the lifespan is expected to contribute to new global efforts to reduce the economic and social costs of TBI and improve access to care for all patients, regardless of their geographical location.”
Dr. Cheryl Wellington, University of British Columbia
The Commission identified substantial disparities in care, including lower treatment intensity for patients injured by low-energy mechanisms, deficiencies in access to rehabilitation and insufficient follow-up in patients with “mild” TBI. In LMICS, both pre-hospital and post-acute care are largely deficient.
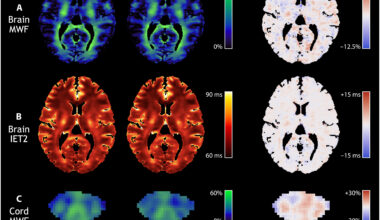
The Commission presents substantial advances in diagnostics and treatment approaches. Blood-based biomarkers perform as well – or perhaps even better – than clinical decision rules for selecting patients with mild TBI for CT scanning, and can thus help reduce unnecessary radiation risks. Moreover, they have prognostic value for outcome. Genomic analyses showed that 26% of outcome variance in TBI might be heritable, emphasizing the relevance of host response, which is modifiable. Advanced monitoring of the brain in patients with severe injuries in the intensive care setting provides better insight into derangements of brain function and metabolism, providing a basis for individualizing management to the needs of a patient. These advances have, however, not (yet) led to improved outcome. Mortality in patients with moderate to severe injuries appears to have decreased, but a greater number of survivors may have substantial disability.
“Traumatic brain injury (TBI) remains a major global health problem, with substantial impact on patients, families and society. Over the last decade, large international collaborations have provided important information to improve understanding and care of TBI. However, significant problems remain, especially in low and middle income countries. Continued collaborative efforts are needed to continue to improve patient outcomes and reduce the societal impact of TBI.”
Prof David K. Menon, University of Cambridge
Despite these advances, many challenges remain and require continued concerted efforts.
Key future research questions in TBI include:
- Why do 50% of mild TBI patients not recover fully? How can we find treatments to address this issue?
- How do we improve treatments for older patients, especially those with comorbidities?
- How does TBI predispose to late-onset neurodegeneration? How can this be treated
- Why do women have poorer outcomes than men following TBI?
- How can we better classify TBI to identify subgroups for individualized treatment?
Addressing these research priorities will be facilitated by:
- Strengthening international collaborative research
- Adopting shared terminology (common data elements) across research studies
- Streamlined regulatory frameworks
- Better incorporation of data science into TBI research
- Engagement with funders, policy makers, regulators, and patient representative groups.